
Cervical osteochondrosis is a type of dystrophic change in the intervertebral discs in the neck.
Not only the discs but also the vertebrae, soft tissues and cartilage are negatively affected. The main feature of the cervical region is the fact that its vertebrae do not have the most reliable structure compared to other regions, which makes this area very vulnerable. The vertebrae are located in close proximity to each other as well as to the arteries that supply the human brain.
If there is a displacement of the vertebrae, then there is a high probability of compression of the nerve bundles and arteries, which will inevitably lead to the appearance of a hernia between the vertebrae and the elongation, d. m. th. changes in the structure of the vertebral disc.
What is it?
Osteochondrosis of the cervical spine (Osteochondrosis) is a degenerative-dystrophic lesion of the intervertebral discs, as a result of which the discs, vertebrae and joints of the cervical spine are damaged and a decrease in the height of the intervertebral discs is observed. . The disease progresses if left untreated and can lead to headaches, poor circulation and even hernias. Like osteoporosis, the disease occurs due to a violation of mineral metabolism, as a result of which the bones and joints become weaker.
Why does osteochondrosis appear?
Although traditional medicine considers degenerative changes in the intervertebral discs of the cervix as a disease, from the point of view of osteopathy, it is only a manifestation of the deepest disorders in the body.
Thus, the real causes of cervical osteochondrosis are:
- Muscle spasms. . . Spasmodic reactions of the muscles of the back, chest, press can lead to the fact that some parts of the body are very tense. As a result, the overall balance position of the body is disturbed, causing a change in the position of the spine. Deformities can affect the cervical region or other parts of the spine, causing osteochondrosis of the chest, cervical and lumbar regions.
- Bad attitude. . . Scoliosis, curvature, rounded back, kyphosis, and other postural disorders, even if minor, cause serious spinal imbalance. As a result, the load on the intervertebral discs is unevenly distributed, which provokes their deformation and increased consumption. The vertebrae begin to converge, causing disruption of nerve processes, osteochondrosis of the cervix develops quite rapidly. Posture disorders caused by a change in the natural position of the ribs have similar consequences.
- Innervation disorder. . . Decreased sensitivity of nerve roots leads to pathological changes in their structure, as a result of which the displacement and deformation of the cervical vertebrae remains unnoticed by the patient. After all, pain is absent due to sensitivity disorders.
- Diseases of the internal organs. . . The wrong position of the internal organs, their displacement and lowering due to various dysfunctions leads to a violation of the overall balance in the body. As a result, it severely affects the position of the spine - the vertebrae of the cervix, lumbar region are displaced and deformed, leading to the corresponding types of osteochondrosis.
- Violation of blood supply. . . Since the vertebral discs have no direct connection to the circulatory system, they receive nourishment from the surrounding tissues. Violation of the blood supply to the cervical spine leads to the fact that the discs do not receive enough fluid for rehydration (restoration of shape due to moisture absorption), rejuvenation of cartilage tissue. As a result, their wear accelerates, there is a decrease in the distance between the vertebrae of the cervical spine, leading to osteochondrosis.
stages
The attending physician should determine the degree of development of cervical osteochondrosis, based on the anamnesis, as well as the examination of the patient. There are only four degrees:
- First step. . . The disease is in the eye, the patient has a slight pain in the neck, which may be stronger if the person begins to turn his head.
- The second degree. . . The patient may complain of very severe pain in the cervical spine, which may be localized in the upper limbs. The clinical picture shows that at this stage of the disease development compression of the nerve bundles is observed, which causes severe pain. Headaches, weakness, and general malaise are also noted.
- Third degree. . . The pain becomes almost uninterrupted, radiating even to the shoulder or arm. Some patients are diagnosed with a disc herniation, which leads to loss of sensation in the upper limbs. On examination by the doctor, there is a noticeable decrease in the mobility of the cervical spine, as well as pain on palpation.
- Fourth degree. . . At this stage of the disease, the intervertebral disc is almost completely destroyed. In its place appears connective tissue, which leads to a deterioration of the patient's condition. He begins to feel more pain, noise in the head, as well as poor orientation in space. This suggests that the artery is constricted, which interferes with the brain's natural nutrition.
The first signs
How is osteochondrosis of the cervical spine manifested:
- radicular syndrome - against the background of compression of nerve endings, pain appears, which spreads from the neck to the edges of the shoulders, forearms, covers the front wall of the chest;
- muscle weakness in the arms, noticeable swelling of the neck;
- when moving the head, a characteristic crack is heard;
- weakness, chronic fatigue, drop in blood pressure;
- lack of coordination, often dizziness, seizures accompanied by nausea, vomiting;
- deterioration of sight and hearing, noise, tinnitus;
- numbness of limbs, tongue;
- frequent migraines;
- in women aged 45-65 years, during sleep there is pain, numbness, tingling in the upper extremities, the attacks may be repeated several times a night.
Symptoms of osteochondrosis of the cervical spine
Important symptoms of cervical osteochondrosis are dizziness, headache, increased blood pressure.
Diagnosis of the disease is difficult, the pain sometimes does not appear and the symptoms disappear, moreover, the uncontrolled use of strong analgesics masks the signs of the disease. A patient who does not feel pain considers himself healthy and this continues until the development of irreversible processes in the tissues of the neck joints.
Headache with cervical osteochondrosis
The most common causes of headache in the pathology we are describing:
- Vascular spasms of the brain;
- Suppressed nerve roots;
- Reflex increase in intracranial pressure.
It feels like the pain can be paroxysmal, constant, throbbing and dull.
Dizziness with cervical osteochondrosis
Dizziness can be caused by:
- Inflammation in the middle or inner ear;
- Vascular spasms of the brain;
- Disorders in the transmission of nerve impulses;
- Problems with the vestibular apparatus;
- Diseases of the cardiovascular system.
There are no clear criteria for dizziness in osteochondrosis. However, there are systemic and non-systematic vertigos, they have obvious differences.
It is recommended to know the differences between systemic and non-systemic dizziness, this will help to independently determine the causes of an unusual condition:
- Systemic dizziness is a sensation of circular motion of objects around or the body, which is a consequence of disruption of the vestibular apparatus, visual analyzers and receptors in the joints, muscles and epidermis (osteochondrosis of various etiologies);
- Unsystematic dizziness is a feeling of dizziness, a feeling of being stunned, insecure about being in an upright position. In the case of unsystematic dizziness, the sensation of circular rotation is absent and this is a significant difference between the compared signs.
A person experiencing dizziness of one of these types should be examined by an experienced physician, primarily a neurologist or (if there is a suspicion of ear and nasopharyngeal disease) by an otolaryngologist.
The reason for urgent hospitalization, which is not associated with osteochondrosis of the cervical spine, is the patient's identification (other than dizziness) of signs such as:
- Facial muscle paralysis and numbness of a part of the shoulder girdle;
- Severe headache against the background of deteriorating health;
- Movement coordination disorders;
- Loss or disappearance of consciousness.
Blood pressure in cervical osteochondrosis
The association of cervical osteochondrosis with increases in blood pressure has long been established. The cervical vertebrae have important nerve endings and blood vessels.
A distinctive feature of high blood pressure in cervical osteochondrosis is a combination of the following symptoms:
- Headache;
- Pain in limbs and chest;
- Decreased sensitivity in the neck area;
- The appearance of increases in pressure after stress, muscle tension, prolonged uncomfortable posture and other similar situations.
These signs should be considered when self-differentiating hypertension of various origins.
Acute spikes in blood pressure and a rapid deterioration in health are the basis for seeking urgent medical help.
Osteochondrosis syndromes
Osteochondrosis consists of the following syndromes:
- Vertebral. . . It is also called vertebral, which indicates that the bones and cartilage tissues are involved in the pathological process. This leads to the formation of such symptoms: restriction of motor activity of the cervix, pain on its return, radiological changes in the image of the cervical spine. Exactly the simultaneous appearance of these signs is vertebral syndrome. A similar set of clinical signs is observed in myositis (muscle tissue pathology), and painful movements accompany many other pathologies.
- Cardiac syndrome. . . Appears with a burning sensation in the chest area, the appearance of shortness of breath. The person feels his or her heart beating fast, becomes tired and irritable. This appearance is also typical for cardiac pathology, for example, for angina pectoris, coronary syndrome, heart attack. An accurate conclusion about the causes of such symptoms can be made after the patient undergoes an ECG.
- Radicular syndrome. . . The cervical region innervates 8 pairs of nerves, each of which has a root - the place where the nerve exits the vertebrae. When involved in osteochondrosis, the patient feels a decrease in sensitivity or vice versa - severe pain. There may be numbness in the neck, if it is painful, decreased sensitivity of the tongue, behind the ear, pain in the supraclavicular region. Sometimes there are swallowing disorders, movement in the upper limb girdle, numbness of the fingers.
Diagnosing
If there are clear signs of cervical osteochondrosis on the face, then the doctor prescribes several methods to make sure the diagnosis is correct:
- X-ray of the cervical spine. This method is advisable in the early stages of the disease, but may be useless in advanced forms.
- CT (computed tomography). This allows you to see structural changes in the vertebrae, but using this method it is impossible to determine the size of the hernia between the vertebrae.
- MRI. It is considered as the most effective diagnostic method in determining cervical osteochondrosis. It is possible to determine the size of the hernia between the discs, as well as the degree of their development.
- Your doctor may also order a duplex scan to determine if your arteries are not working properly.
Complications of the disease
What is the risk of cervical osteochondrosis:
- frequent migraine attacks;
- heart rhythm disorders, atherosclerosis;
- elongation, intervertebral hernia, vertebral bone growth;
- serious brain pathology;
- narrowing of the lumen of the vertebral artery, which leads to the development of VSD, cerebral hypertension, disability;
- stroke in the spine.
First aid at home with the worsening of osteochondrosis
For severe pain, pain relievers may be used. If analgesics do not provide relief, NSAIDs may be taken.
Often used "distracting" means, for example, plaster with peppers, which does not heal, but only warms the inflamed area and distracts from the pain. In case of edema in the area of inflammation, the patient can drink an herbal infusion or a diuretic for 3-4 days. Can osteochondrosis be cured by such methods? These measures are only temporary, to treat the causes, you should consult a doctor.
How to treat osteochondrosis of the cervical spine?
In the initial stage of development, osteochondrosis can be cured without medication, it is enough to review your diet, daily regimen and regularly perform a series of special exercises. With advanced forms of the disease, effective treatment is possible only with the use of various medications that help stop the degenerative changes in the vertebrae.
The complex of therapeutic measures should include physiotherapy - electrophoresis with drugs, ultrasound, magnetotherapy, laser therapy. These methods help to cope with pain, inflammation, swelling of tissues, improve metabolic processes and blood circulation.
Drug treatment
The main methods of treating osteochondrosis of the cervix are medication, physiotherapy, massage of the cervical area, therapeutic exercises for cervical osteochondrosis are particularly effective. The main groups of drugs used for this disease include:
| Name | Principle of operation |
| Non-steroidal anti-inflammatory drugs (NSAIDs). | They reduce pain, help relieve aseptic inflammation and edema of the damaged nerve root. |
| Drugs that improve the rheological properties of blood and blood flow. | Improves nutrition of damaged nerve roots and improves blood flow to the brain. |
| vitamin B. | Improves metabolic processes in nerve tissue. |
| Muscle relaxants. | These are drugs that relieve muscle spasms. |
| Chondroprotectors. These are glucosamine and chondroitin. | These are drugs that restore cartilage tissue, including damaged intervertebral discs. |
When taking osteochondrosis pills, it should be remembered that a significant effect of pill medication treatment will only be if you combine it with other methods, including exercise. It should also be noted that the attending physician should prescribe the treatment of the disease based on its stage and other signs.
Many doctors consider it effective to treat osteochondrosis of the cervix with injections, as this allows faster action on the nerve endings and causes a minimum of side effects. At the same time, vitamins are best taken in pill form, as there is no change for assimilation, but injections can be painful.
Injections used for treatment:
- intramuscular injections cause a general tonic and anti-inflammatory effect;
- blockages are injected directly into the affected area, which leads to a rapid effect.
Ointments and gels for external use
This is the most accessible group of medicines for home use. They are divided into inflammation relievers, warmers and pain relievers.
With cervical osteochondrosis, not all oils are effective, in addition, due to their availability, they are sometimes used unreasonably and regardless of the features of pathogenesis. Before using any medication, you should be examined by a doctor.
Exercise therapy
Physiotherapy for cervical osteochondrosis should be performed without acute exacerbation. The greatest efficiency of this technique is during the recovery period. There should be no discomfort and pain during the execution of the complex!
| Exercise number 1 | Lying on your stomach, place your hands on the floor, raise your head and torso, your back should be straight. Stay in this position for 1-2 minutes. Slowly lower yourself to the floor. Repeat 2-3 times. |
| Exercise number 2 | Lying on your stomach, spread your arms along your body, turn your head to the left, try to touch the floor with your ear, and then turn your head to the right. Repeat 6-7 times in each direction. |
| Exercise number 3 | In a sitting position, while inhaling, lean forward and try to touch the chest with your head, then exhale, lean back and tilt your head back. Repeat 10-15 times. |
| Exercise number 4 | While sitting, place your palms on your forehead, apply pressure with your palms to your forehead and forehead to your palms. Continue this exercise for 30 seconds. Repeat 2-3 times. |
| Exercise number 5 | Slowly rotate the head first in one direction, then in the other. 10 turns in each direction. Beware of dizziness. When it appears, the exercise stops. |

Massage for osteochondrosis of the cervix
The massage should be done carefully, without straining. Inexperienced and unprofessional massage can end in failure. The movements should extend to the cervical region, the collar area and part of the back. The massage is performed in a supine position, in extreme cases, in a sitting position.
The techniques are based on the following techniques:
- Ledhatimi. Impact on the surface layers of the skin. With the palms of the hands or the tips of the fingers from the head down to the upper third of the middle of the back. The kick from the base of the neck can also be in a zigzag pattern;
- Squeeze. Impact on the deeper layers of the skin in the upper third of the back. The fingers (thumb and forefinger) along the neck make movements to catch the skin, reminiscent of tightening. This is done carefully, the tissues near the vertebrae are not involved;
- Triturimi. The purpose of the procedure is to warm the skin and increase blood circulation to the neck area. This is done with extreme caution. Influence on the spinous processes of the vertebrae is not allowed. Friction can be replaced with movements reminiscent of sawing, or circular stroking;
- Decoction. It has a limited importance, as it affects very deep tissues, which can worsen the pathology.
Self-massage for cervical osteochondrosis is performed while you are sitting in a comfortable position. Methods of hitting, circular rubbing on the neck or shoulders are used. It is advisable to combine the method of self-massage with rubbing with different ointments that increase blood circulation and relieve pain in the kneaded area.

Physiotherapy
Along with taking the medication, the patient should undergo physiotherapy procedures. They increase the effectiveness of drugs and promote the restoration of joints and intervertebral discs.
- Electrophoresis - ions of anesthetic drug penetrate the injured site due to the action of an electric current.
- Laser therapy - has anti-inflammatory properties, guarantees an improvement of blood circulation, through exposure to light.
- Magnetic therapy - relieves swelling of tissues, has an analgesic effect.
- Ultrasound - has an improvement in metabolic processes, pain relief, relieving inflammation of damaged areas.
Several procedures are used in the form of physiotherapy. The doctor prescribes treatment, relying on the indications and the absence of contraindications.

Folk remedies
Alternative treatment should be used as an adjunct to drug therapy and physical education, unconventional methods will not help to completely get rid of the disease.
What to do with cervical osteochondrosis at home:
- Pour boiling water over a fresh horseradish leaf, cool slightly, stick the inside to the neck, fix with a thin natural cloth. The procedure is done before going to bed, leave the compress on overnight.
- Grind the raw potatoes on a fine grater, mix in equal proportions with warm liquid honey. Use the mixture for compresses, the procedure should be performed 1-2 times a week.
- Mix a raw egg with 100 ml of sunflower oil, 20 ml of vinegar and 20 g of flour, remove the mixture in a dark place for 48 hours, remove the film from the surface. Tools to paint the inflamed area before going to bed, store in the refrigerator.
- In May, collect pine buds up to 2 cm long, cut into thin slices, fold in a dark glass container. For 1 part of raw material, take 2 parts of sugar, remove the drug in a dark place for 2 weeks. Drink 5 ml of the mixture three times a day, do not swallow immediately, keep in the mouth for 2-3 minutes. Course duration - 15-20 days, repeated 2-3 times a year.
- Grind 150 gr of peeled garlic and 400 gr of cranberry, place the mixture in a glass container, add 800 ml of honey after 24 hours, mix. Take 5 ml of the drug three times daily before meals.
Face the severe pain, remove excess salts with a cabbage leaf dyed with honey, arrange the compress on the neck with a warm scarf, leave overnight.
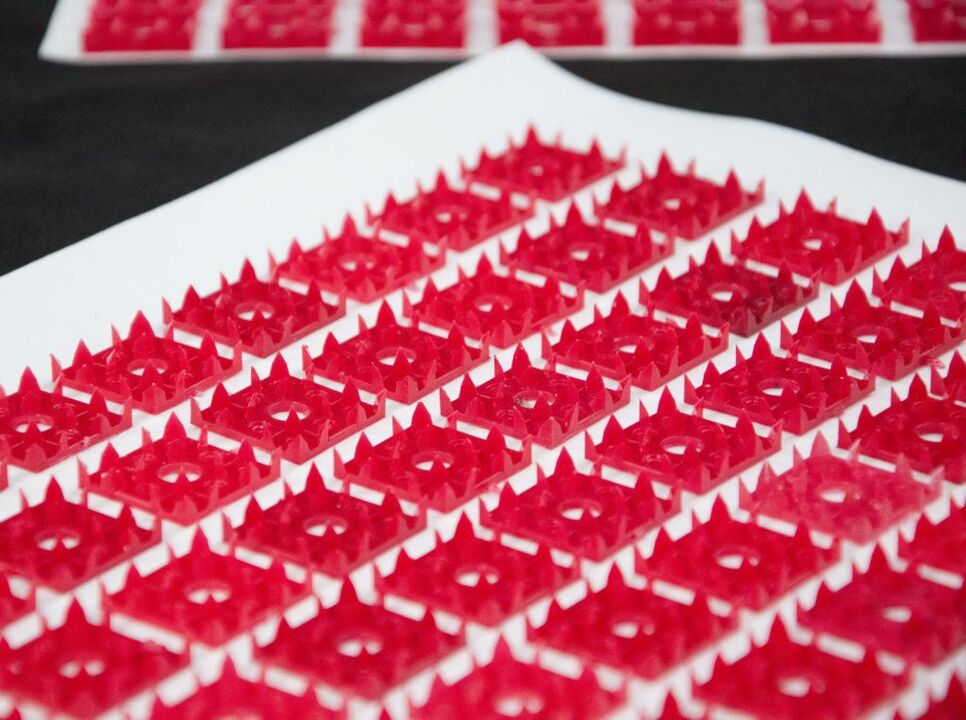
applicator
The use of applicators is one of the methods of therapy for spinal diseases, including osteochondrosis.
The impact of the device on the cervical spine normalizes metabolic processes, relieves pain, increases muscle tone, improves blood circulation, increases the conduction of nerve tissue, etc.
Manual therapy
Manual therapy is based on the principle of restoring motor functions and mobility between the vertebrae.
Initially the manipulations consist of a lightly relaxing massage, then the doctor exercises more and more force, acts on the vertebrae by pressing and turning the neck.

Surgery
The back is the foundation of the whole human body. When diagnosing any pathology related to the spine, specialists seek to eliminate it therapeutically. Any operation on the spine is life threatening.
With osteochondrosis of the cervix, surgery is allowed under the following indications:
- intervertebral hernia, spondylolisthesis, spinal stenosis;
- lack of therapy results when exposed for more than six months;
- osteophyte formation.
Modern medicine offers many ways to perform surgeries with minimal risks to the health and life of the patient.
Prophylaxis
Osteochondrosis of the cervix is a disease that develops, first of all, with an improper lifestyle. Therefore, disease prevention is a healthy lifestyle.
It is possible to reduce the risk of developing OCD if:
- exclude provocative factors;
- exercise regularly;
- do not engage in strenuous physical activity;
- give up bad habits;
- try to be as nervous as possible;
- eat properly.
Compliance with preventive measures will help speed up the healing process and eliminate the likelihood of relapse. The elderly and those with a hereditary predisposition are advised to consistently adhere to prevention. Compliance with a diet, performing simple exercises will definitely bring a positive result. It is also useful for doing yoga and swimming.



















